

Staying compliant with the Health Insurance Portability and Accountability Act (HIPAA) is a non-negotiable, continuous responsibility for all organizations that handle protected health information (PHI). A common mistake most organizations make is treating compliance as a one-time task rather than an ongoing commitment.
You can avoid the risk of falling out of HIPAA compliance by integrating key workflows into your organization’s security and operational strategy. This guide will help you understand:
- Why HIPAA requires ongoing compliance
- What requirements you must meet
We’ll also cover six best practices that help you maintain ongoing HIPAA compliance.
Why HIPAA requires ongoing compliance
HIPAA is a federal law that sets strict standards for how organizations use and manage protected health information (PHI).
Since its enactment in 1996, HIPAA has evolved to address changes in the security landscape, covering emerging security threats and new technologies. Because of this, organizations must regularly review and update their policies, procedures, and safeguards to stay aligned with the latest HIPAA requirements.
Another reason why organizations in scope are expected to maintain compliance at all times is the high security risk involved—and the potential for unannounced audits.
To ensure compliance, the Office for Civil Rights (OCR), the federal agency responsible for enforcing HIPAA, can launch audits or investigations into covered entities without prior notice. These actions can be triggered by patient complaints, breach reports, or chances of elevated risks. That’s why all organizations under HIPAA’s scope, including covered entities and the business associates they partner with, must be audit-ready at all times.
Covered entities can also exercise their right to audit business associates at any moment to verify if the appropriate safeguards outlined in the business associate agreement (BAA) are in place.
Failing to meet HIPAA requirements can lead to significant consequences, including:
- Corrective measures
- Financial penalties
- Legal escalation
- Contract termination (for business associates and contractors)
Key requirements for ongoing HIPAA compliance
Ongoing HIPAA compliance is primarily governed by the Security and Privacy rules. Both set the standards that organizations must implement to protect the integrity and confidentiality of PHI.
To stay compliant, covered entities and business associates must meet several core requirements to avoid mistakes or unintentional violations. Their key responsibilities include:
- Conducting access control reviews: Organizations need to regularly review who is authorized to view and access PHI.
- Performing security audits: Entities should systematically evaluate technical and physical safeguards to protect PHI.
- Carrying out risk assessments: HIPAA requires periodic risk assessments to identify, document, and mitigate threats to PHI.
- Updating and reviewing policies: You must adjust policies and procedures to keep up with regulatory updates and technological changes. In fact, in a recent Vanta survey, 41% of organizations reported evolving regulations as their top challenge for staying HIPAA compliant.
- Retaining compliance-related documentation: HIPAA requires that all documentation about compliance (like policies, breach logs, training logs, and other records) be retained for a minimum of six years to support accountability and ensure audit-readiness.
While HIPAA does not prescribe the frequency for self-attestation, the Department of Health and Human Services (HHS) as well as industry standards recommend conducting key compliance activities, such as risk assessments, employee training, and policy reviews, at least annually. However, this annual cadence should be considered a minimum baseline—ongoing compliance may require more frequent check-ins.
{{cta_withimage13="/cta-blocks"}} | HIPAA compliance checklist
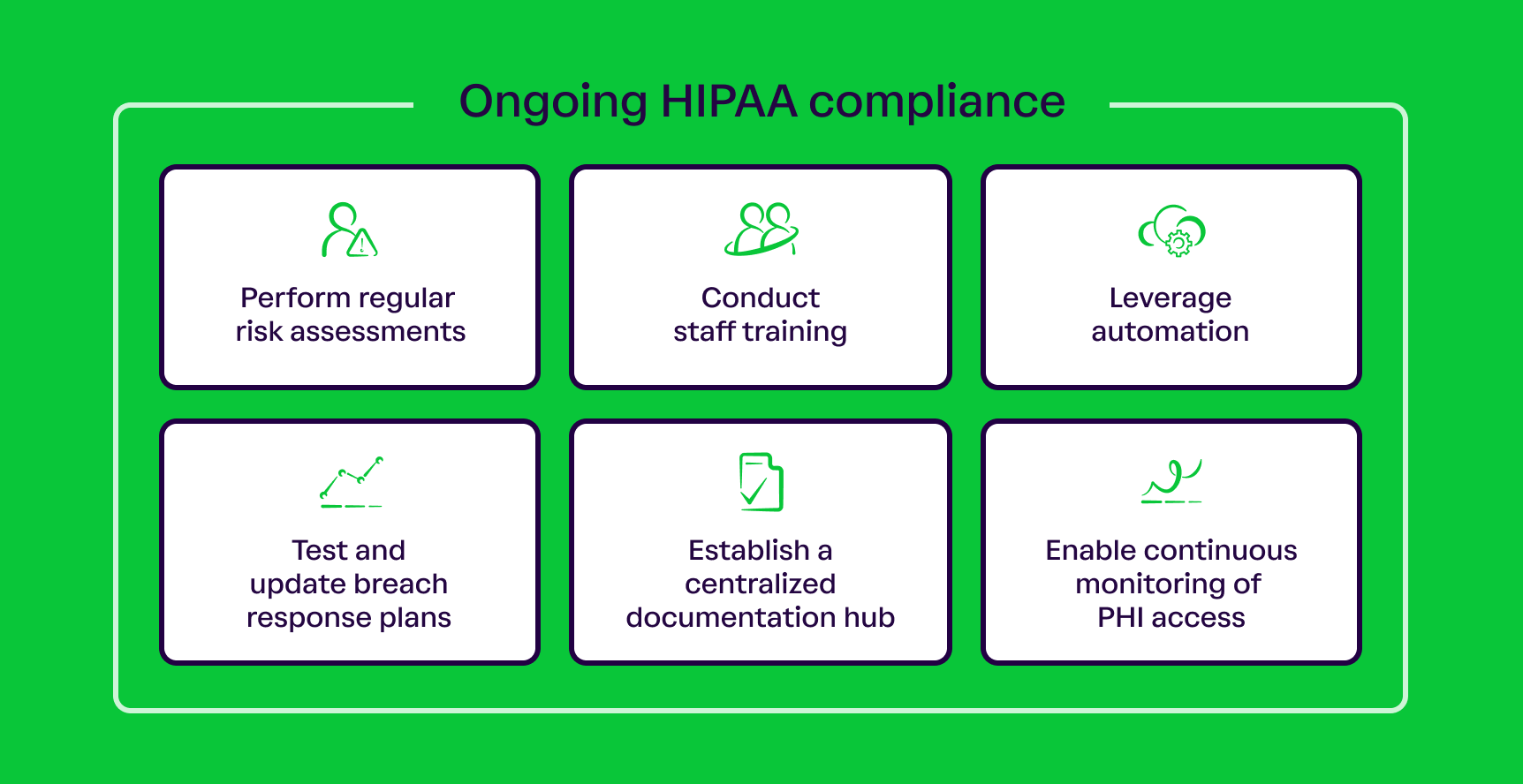
6 best practices for ongoing HIPAA compliance
To maintain compliance despite all the challenges, you should adopt the following best practices for long-term HIPAA compliance:
- Perform regular risk assessments
- Conduct staff training
- Enable continuous monitoring of PHI access
- Establish a centralized documentation hub
- Test and update breach response plans
- Leverage automation
1. Perform regular risk assessments
Conducting a regular and thorough risk assessment is a foundational requirement of the HIPAA Security Rule—and a foundational aspect of ongoing compliance. A comprehensive risk assessment typically involves:
- Identifying potential threats and vulnerabilities across systems
- Evaluating the likelihood and potential impact of scenarios like unauthorized access
- Creating a risk mitigation plan with timelines, corrective actions, and task owners
- Reviewing the efficacy of existing safeguards
These assessments are not only a core step for maintaining compliance but also serve as a proactive method for identifying and addressing vulnerabilities.
Even though the Security Rule focuses on electronic PHI (ePHI), the risk assessment should also evaluate physical PHI and related assets for comprehensive coverage.
2. Conduct staff training
Your workforce is the first line of defense when it comes to safeguarding PHI across everyday operations. That makes proper staff training crucial for ongoing compliance. According to Vanta’s 2025 survey, 83% of organizations already offer HIPAA-specific compliance training to employees.
Ensure your staff members understand HIPAA basics, such as:
- What HIPAA policies are
- How to identify PHI
- How to safeguard PHI
- How to report potential breaches
You should share real-world examples that show the consequences of PHI leaks as part of the training. Teaching about the impact of mishandling PHI will help build accountability in your team.
Maintain a consistent training schedule for your team, and hold additional sessions after security incidents, regulatory updates, technical changes, and other disruptive events.
3. Enable continuous monitoring of PHI access
Monitoring who can access PHI is relevant for both compliance and data security. The HIPAA Security Rule requires organizations to track and log access to ePHI, such as:
- User identity
- Time and date of access
- Successful and failed login attempts
- Specific files that have been accessed
Gaps in the process can delay breach detection, response, and notification to the affected parties, which increases the risk of violating the Breach Notification Rule.
Continuous monitoring of PHI can be implemented through real-time alerts for suspicious activities, tracking user logins, and periodic reports for compliance reviews.
Avoid manual logging of PHI access if you want to maintain ongoing compliance easily. In such cases, you’d have to assign someone to monitor the spreadsheets or logs every day, which makes the incident detection system slow and error-prone. Such lapses in monitoring and accountability can be avoided by implementing automation software to track PHI from a singular dashboard.
4. Establish a centralized documentation hub
As mentioned earlier, the HIPAA Security and Privacy rules mandate that organizations maintain comprehensive documentation such as access logs, breach records, BAAs, and risk assessment results. However, many of these documents are stored in different systems across departments, making it difficult for IT and compliance teams to conduct validations or collect evidence for future audits.
Another challenge is meeting the six-year documentation retention rule. When HIPAA records are scattered or stored in non-searchable formats, it can slow down ongoing monitoring procedures. For instance, retrieving or referencing records during an investigation or audit could get challenging.
A centralized documentation software addresses these challenges by streamlining record-keeping and making tracking across large volumes of documents easier with minimal administrative overhead.
{{cta_withimage39="/cta-blocks"}} | The Healthcare compliance checklist
5. Test and update breach response plans
The Breach Notification Rule outlines strict timelines and procedures for reporting a breach of unsecured PHI. Specifically, covered entities must notify affected individuals and HHS no later than 60 days from the discovery of the breach. It might not seem like a tight deadline, but processes like risk assessment and system investigation easily fit into the window.
Your ongoing compliance process should include regular testing of your organization’s response capabilities. Simulation exercises can help you evaluate your response plans and procedures, clarify team roles, and reveal potential flaws.
Once you update your breach response plans, you may want to stress-test them again after an interval, with the cadence depending on your organization's risk landscape. The goal is to help your team react quickly, with clarity and confidence in their actions.
6. Leverage automation
Maintaining HIPAA compliance involves complex workflows that can overwhelm IT, security, and compliance teams, especially when handled manually. Issues such as delayed incident responses, operational disruptions, and poor visibility into compliance status can increase the risk of PHI breaches and drain time and resources for busy teams.
To prevent these bottlenecks, consider leveraging automation software purpose-built for HIPAA compliance. Automated solutions can eliminate most of the manual work involved in recurring workflows like documentation collection, control monitoring, and evidence gathering. This can accelerate the compliance process, reduce human error, and free up your team's time so they can focus on higher-value tasks.
Stay HIPAA compliant with Vanta
Vanta is a trust management and GRC platform designed to help you maintain HIPAA compliance with minimal time and resource investment. The platform can automate numerous HIPAA workflows, which makes compliance more manageable.
Vanta’s HIPAA suite is designed for both initial and continuous compliance. Its clear guidance and built-in resources for controls, policies, and documentation can reduce the overhead for your security and compliance teams.
Once you become HIPAA-compliant, you can monitor and maintain your compliance health with features such as:
- Real-time monitoring and instant security reports
- Integration with 375+ business tools for collecting evidence
- Built-in training for staff
- Drafting and tracking BAAs
- A real-time dashboard for tracking
If you’re already compliant with other frameworks such as HITRUST, ISO 27001, and SOC 2, or you aim to be, Vanta’s cross-mapping feature can help you reuse any overlapping controls and achieve compliance faster. The platform supports over 35 frameworks, helping you maintain your compliance posture across industries and at any scale.
Schedule a free demo today and find out how Vanta can simplify your compliance efforts.
{{cta_simple18="/cta-blocks"}} | HIPAA product page
A note from Vanta: Vanta is not a law firm, and this article does not constitute or contain legal advice or create an attorney-client relationship. When determining your obligations and compliance with respect to relevant laws and regulations, you should consult a licensed attorney.
Streamlining HIPAA compliance
Best practices for ongoing HIPAA compliance

Looking to streamline the work for HIPAA compliance?
Staying compliant with the Health Insurance Portability and Accountability Act (HIPAA) is a non-negotiable, continuous responsibility for all organizations that handle protected health information (PHI). A common mistake most organizations make is treating compliance as a one-time task rather than an ongoing commitment.
You can avoid the risk of falling out of HIPAA compliance by integrating key workflows into your organization’s security and operational strategy. This guide will help you understand:
- Why HIPAA requires ongoing compliance
- What requirements you must meet
We’ll also cover six best practices that help you maintain ongoing HIPAA compliance.
Why HIPAA requires ongoing compliance
HIPAA is a federal law that sets strict standards for how organizations use and manage protected health information (PHI).
Since its enactment in 1996, HIPAA has evolved to address changes in the security landscape, covering emerging security threats and new technologies. Because of this, organizations must regularly review and update their policies, procedures, and safeguards to stay aligned with the latest HIPAA requirements.
Another reason why organizations in scope are expected to maintain compliance at all times is the high security risk involved—and the potential for unannounced audits.
To ensure compliance, the Office for Civil Rights (OCR), the federal agency responsible for enforcing HIPAA, can launch audits or investigations into covered entities without prior notice. These actions can be triggered by patient complaints, breach reports, or chances of elevated risks. That’s why all organizations under HIPAA’s scope, including covered entities and the business associates they partner with, must be audit-ready at all times.
Covered entities can also exercise their right to audit business associates at any moment to verify if the appropriate safeguards outlined in the business associate agreement (BAA) are in place.
Failing to meet HIPAA requirements can lead to significant consequences, including:
- Corrective measures
- Financial penalties
- Legal escalation
- Contract termination (for business associates and contractors)
Key requirements for ongoing HIPAA compliance
Ongoing HIPAA compliance is primarily governed by the Security and Privacy rules. Both set the standards that organizations must implement to protect the integrity and confidentiality of PHI.
To stay compliant, covered entities and business associates must meet several core requirements to avoid mistakes or unintentional violations. Their key responsibilities include:
- Conducting access control reviews: Organizations need to regularly review who is authorized to view and access PHI.
- Performing security audits: Entities should systematically evaluate technical and physical safeguards to protect PHI.
- Carrying out risk assessments: HIPAA requires periodic risk assessments to identify, document, and mitigate threats to PHI.
- Updating and reviewing policies: You must adjust policies and procedures to keep up with regulatory updates and technological changes. In fact, in a recent Vanta survey, 41% of organizations reported evolving regulations as their top challenge for staying HIPAA compliant.
- Retaining compliance-related documentation: HIPAA requires that all documentation about compliance (like policies, breach logs, training logs, and other records) be retained for a minimum of six years to support accountability and ensure audit-readiness.
While HIPAA does not prescribe the frequency for self-attestation, the Department of Health and Human Services (HHS) as well as industry standards recommend conducting key compliance activities, such as risk assessments, employee training, and policy reviews, at least annually. However, this annual cadence should be considered a minimum baseline—ongoing compliance may require more frequent check-ins.
{{cta_withimage13="/cta-blocks"}} | HIPAA compliance checklist
6 best practices for ongoing HIPAA compliance
To maintain compliance despite all the challenges, you should adopt the following best practices for long-term HIPAA compliance:
- Perform regular risk assessments
- Conduct staff training
- Enable continuous monitoring of PHI access
- Establish a centralized documentation hub
- Test and update breach response plans
- Leverage automation
1. Perform regular risk assessments
Conducting a regular and thorough risk assessment is a foundational requirement of the HIPAA Security Rule—and a foundational aspect of ongoing compliance. A comprehensive risk assessment typically involves:
- Identifying potential threats and vulnerabilities across systems
- Evaluating the likelihood and potential impact of scenarios like unauthorized access
- Creating a risk mitigation plan with timelines, corrective actions, and task owners
- Reviewing the efficacy of existing safeguards
These assessments are not only a core step for maintaining compliance but also serve as a proactive method for identifying and addressing vulnerabilities.
Even though the Security Rule focuses on electronic PHI (ePHI), the risk assessment should also evaluate physical PHI and related assets for comprehensive coverage.
2. Conduct staff training
Your workforce is the first line of defense when it comes to safeguarding PHI across everyday operations. That makes proper staff training crucial for ongoing compliance. According to Vanta’s 2025 survey, 83% of organizations already offer HIPAA-specific compliance training to employees.
Ensure your staff members understand HIPAA basics, such as:
- What HIPAA policies are
- How to identify PHI
- How to safeguard PHI
- How to report potential breaches
You should share real-world examples that show the consequences of PHI leaks as part of the training. Teaching about the impact of mishandling PHI will help build accountability in your team.
Maintain a consistent training schedule for your team, and hold additional sessions after security incidents, regulatory updates, technical changes, and other disruptive events.
3. Enable continuous monitoring of PHI access
Monitoring who can access PHI is relevant for both compliance and data security. The HIPAA Security Rule requires organizations to track and log access to ePHI, such as:
- User identity
- Time and date of access
- Successful and failed login attempts
- Specific files that have been accessed
Gaps in the process can delay breach detection, response, and notification to the affected parties, which increases the risk of violating the Breach Notification Rule.
Continuous monitoring of PHI can be implemented through real-time alerts for suspicious activities, tracking user logins, and periodic reports for compliance reviews.
Avoid manual logging of PHI access if you want to maintain ongoing compliance easily. In such cases, you’d have to assign someone to monitor the spreadsheets or logs every day, which makes the incident detection system slow and error-prone. Such lapses in monitoring and accountability can be avoided by implementing automation software to track PHI from a singular dashboard.
4. Establish a centralized documentation hub
As mentioned earlier, the HIPAA Security and Privacy rules mandate that organizations maintain comprehensive documentation such as access logs, breach records, BAAs, and risk assessment results. However, many of these documents are stored in different systems across departments, making it difficult for IT and compliance teams to conduct validations or collect evidence for future audits.
Another challenge is meeting the six-year documentation retention rule. When HIPAA records are scattered or stored in non-searchable formats, it can slow down ongoing monitoring procedures. For instance, retrieving or referencing records during an investigation or audit could get challenging.
A centralized documentation software addresses these challenges by streamlining record-keeping and making tracking across large volumes of documents easier with minimal administrative overhead.
{{cta_withimage39="/cta-blocks"}} | The Healthcare compliance checklist
5. Test and update breach response plans
The Breach Notification Rule outlines strict timelines and procedures for reporting a breach of unsecured PHI. Specifically, covered entities must notify affected individuals and HHS no later than 60 days from the discovery of the breach. It might not seem like a tight deadline, but processes like risk assessment and system investigation easily fit into the window.
Your ongoing compliance process should include regular testing of your organization’s response capabilities. Simulation exercises can help you evaluate your response plans and procedures, clarify team roles, and reveal potential flaws.
Once you update your breach response plans, you may want to stress-test them again after an interval, with the cadence depending on your organization's risk landscape. The goal is to help your team react quickly, with clarity and confidence in their actions.
6. Leverage automation
Maintaining HIPAA compliance involves complex workflows that can overwhelm IT, security, and compliance teams, especially when handled manually. Issues such as delayed incident responses, operational disruptions, and poor visibility into compliance status can increase the risk of PHI breaches and drain time and resources for busy teams.
To prevent these bottlenecks, consider leveraging automation software purpose-built for HIPAA compliance. Automated solutions can eliminate most of the manual work involved in recurring workflows like documentation collection, control monitoring, and evidence gathering. This can accelerate the compliance process, reduce human error, and free up your team's time so they can focus on higher-value tasks.
Stay HIPAA compliant with Vanta
Vanta is a trust management and GRC platform designed to help you maintain HIPAA compliance with minimal time and resource investment. The platform can automate numerous HIPAA workflows, which makes compliance more manageable.
Vanta’s HIPAA suite is designed for both initial and continuous compliance. Its clear guidance and built-in resources for controls, policies, and documentation can reduce the overhead for your security and compliance teams.
Once you become HIPAA-compliant, you can monitor and maintain your compliance health with features such as:
- Real-time monitoring and instant security reports
- Integration with 375+ business tools for collecting evidence
- Built-in training for staff
- Drafting and tracking BAAs
- A real-time dashboard for tracking
If you’re already compliant with other frameworks such as HITRUST, ISO 27001, and SOC 2, or you aim to be, Vanta’s cross-mapping feature can help you reuse any overlapping controls and achieve compliance faster. The platform supports over 35 frameworks, helping you maintain your compliance posture across industries and at any scale.
Schedule a free demo today and find out how Vanta can simplify your compliance efforts.
{{cta_simple18="/cta-blocks"}} | HIPAA product page
A note from Vanta: Vanta is not a law firm, and this article does not constitute or contain legal advice or create an attorney-client relationship. When determining your obligations and compliance with respect to relevant laws and regulations, you should consult a licensed attorney.
Explore more HIPAA articles
Introduction to HIPAA
HIPAA requirements
Preparing for HIPAA compliance
Streamlining HIPAA compliance
Get started with HIPAA:
Start your HIPAA journey with these related resources.

An 8-step HIPAA compliance checklist to meet privacy and security requirements
Use this handy HIPAA compliance checklist to ensure adherence to the key requirements.

HIPAA violations in 2025: Staff mistakes and vendor blind spots
Discover what a HIPAA violation is, common causes behind violations
Live Demo: Automating Compliance for SOC 2, ISO 27001, HIPAA, and More
Discover how Vanta’s automation and AI tools can help your team simplify compliance, strengthen security, and scale trust across frameworks like SOC 2, ISO 27001, HIPAA, and more.




