

The Health Insurance Portability and Accountability Act (HIPAA) is a U.S. federal law that came into force in 1996, with the ultimate goal to establish standards for protecting sensitive patient information. The regulation primarily applies to organizations that handle protected health information (PHI), which refers to a patient’s individually identifiable information collected or generated during treatment.
Since HIPAA compliance is mandatory for many organizations in healthcare, avoiding the related fines is enough of an incentive to invest in compliance.
However, organizations not legally obligated to follow the regulation are also considering compliance. These are organizations looking to enter regulated markets and want to demonstrate optimized security systems or operations to stakeholders or justify the resources HIPAA demands to leadership.
In this guide, we’ll look at seven benefits of pursuing HIPAA compliance—with these, you’ll be able to assess HIPAA’s value for your organization and build a case to get the necessary buy-in from stakeholders.
Who needs to comply with HIPAA and why it matters
Today, any organization that stores, maintains, or transmits PHI must comply with HIPAA.
HIPAA’s original goal was to improve health insurance portability by ensuring that individuals don’t lose coverage between jobs, particularly if they have pre-existing health conditions. Over time, the law has expanded to include federal standards for safeguarding sensitive patient information.
These additional measures put increased financial pressure on insurers, which could be passed on to customers. To address these issues, the Department of Health and Human Services (HHS) established standards aimed at reducing administrative strain and codifying the rules for handling PHI. These rules were originally developed for covered entities, which include:
- Healthcare providers
- Health plans
- Healthcare clearinghouses
The HITECH Act in 2009 broadened HIPAA’s scope to include business associates, which are organizations that enter business associate agreements (BAAs) with covered entities and handle PHI on their behalf.
Organizations that fail to comply with HIPAA can face serious consequences. The HHS Office for Civil Rights (OCR) evaluates violations based on their severity and intent, and may impose different penalties, including corrective actions, financial penalties, or even criminal charges.
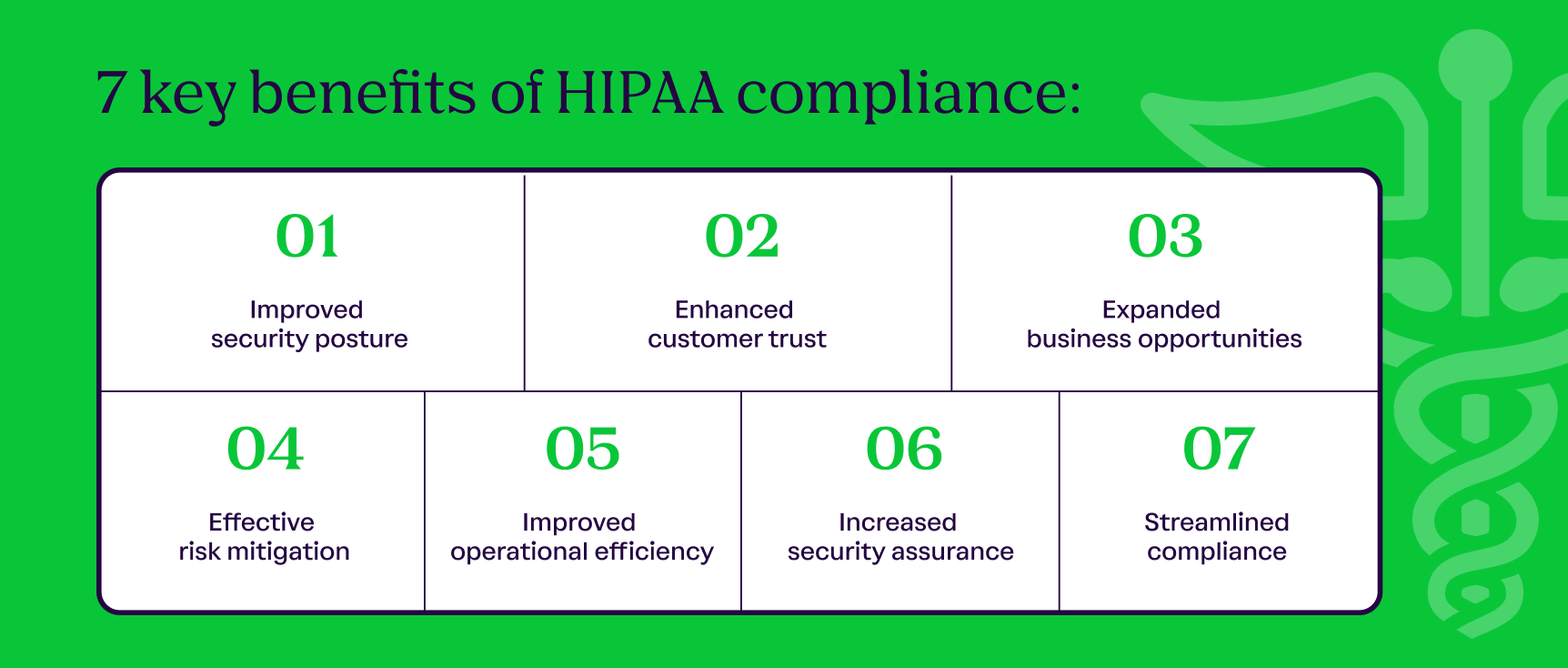
7 key benefits of HIPAA compliance
Achieving ongoing HIPAA compliance—mandatory or otherwise—provides several notable benefits to your organization, including:
- Improved security posture
- Enhanced customer trust
- Expanded business opportunities
- Effective risk mitigation
- Improved operational efficiency
- Increased security assurance
- Streamlined compliance
1. Improved security posture
The most significant benefit of HIPAA compliance is an improved security posture. Since HIPAA's core objective is to protect sensitive health information, it requires organizations to implement several key security practices, including:
- Encryption
- Access control
- Data minimization
- Audit trails
HIPAA also strengthens your security posture by enabling rigorous testing and assessments. You'll conduct thorough reviews as part of the preparation process, so you’ll know how effective your security controls are.
The HIPAA Security Rule also emphasizes the need for regular reviews, which you can achieve through continuous monitoring. That way, you’ll be able to stay up-to-date with evolving security practices efficiently, and minimize gaps and non-compliance risk.
Keeping up with regulatory changes becomes particularly important following the 2025 updates to the Security Rule, aimed at making security requirements significantly more prescriptive. Some notable updates include areas such as:
- Risk analysis
- Encryption
- Inventory management
- Multifactor authentication
- Third-party risk management
{{cta_withimage13="/cta-blocks"}} | HIPAA compliance checklist
2. Enhanced customer trust
HIPAA is one of the oldest and most commonly used security standards in the healthcare industry. Demonstrating compliance with it is an effective way of showing your organization’s dedication to data security and privacy, enhancing partner and customer trust.
The framework implements multiple industry-best measures that overlap with several other leading frameworks, such as:
This overlap means that compliance with HIPAA will give you a head start when pursuing other frameworks to enhance customer trust. For instance, you can achieve SOC 2 attestation or NIST certification faster to demonstrate security to a lead and expedite the deal cycle.
3. Expanded business opportunities
HIPAA compliance can be valuable even if you haven’t yet entered the healthcare market or want to explore a new market segment. Demonstrating that you meet all of the regulation’s requirements can help you secure contracts even as a fairly new startup.
HIPAA compliance can also benefit organizations outside the healthcare sector. Aligning with an industry-leading standard can give your organization a competitive edge in other industries where data protection is critical, such as finance, SaaS, or online media.
Additionally, HIPAA may boost your eligibility to win certain government contracts, especially those involving health data or requiring strong privacy practices to protect personally identifiable information (PII). While HIPAA-aligned controls won’t tick off government requirements automatically, they can help streamline the qualification process and demonstrate a strong baseline of security.
4. Effective risk mitigation
Conducting regular risk assessments is a core requirement of continuous HIPAA compliance. Frequent evaluations provide better insights into the effectiveness of your existing controls and help identify potential issues before they escalate.
Proactive measures are particularly important for compliance with the Breach Notification Rule. Under this rule, when a covered entity experiences a security incident involving unsecured PHI, it must notify the HHS and affected individuals within strict timeframes.
Even if your organization isn’t in the healthcare industry, strict breach reporting requirements highlight the importance of taking proactive measures and implementing an effective incident response plan.
Regular assessments will also help you manage third-party risk more effectively. According to HIPAA, you’ll have to consider vendor risk for third parties like business associates as part of your mitigation plans, which helps maintain a clear audit trail.
5. Improved operational efficiency
One of the main ideas behind HIPAA is streamlining operational and administrative processes for covered entities. To achieve this, the framework introduces standardized procedures and protocols under the Security and Privacy rules.
For example, the Privacy Rule requires organizations to implement strict guidelines for disclosing PHI, train employees how to follow them, and share only the minimum amount of information needed for a specific purpose.
The Security Rule focuses on safeguarding electronic PHI by requiring access control, audit logging, and incident response protocols. This rule also specifies the requirements that need to be outlined in business associate agreements, which you can use to streamline your third-party risk management efforts.
Following an established set of controls helps you maintain your security posture efficiently and minimizes the risk of uneven implementation between departments.
6. Increased security assurance
HIPAA does not offer an official certificate for compliance, unlike many other frameworks. As a federal regulation, HIPAA requires all in-scope organizations to comply, regardless of whether they've completed an external audit or assessment.
Organizations looking to demonstrate compliance to third parties can still do so by completing one of two types of assessments:
- Self-assessments conducted by internal teams to evaluate compliance with HIPAA requirements
- Third-party assessments performed by an independent consultant or auditor to provide external validation
Although self-assessments may be more straightforward, an independent auditor brings objective insight on how well your organization has implemented the required controls, providing additional confidence in your security posture.
If your organization handles PHI, you may also be subject to HHS audits. These are performed by the OCR to evaluate whether you meet the requirements for the Security, Privacy, and Breach Notification rules. An audit may happen at random or following a breach or complaint.
HHS audits are enforcement activities—unlike self- and third-party assessments, violations may result in corrective action or fines. That’s why HIPAA specifically mandates compliance-related documentation must be retained for a minimum of six years, as it’s a key part of demonstrating compliance during an HHS audit.
{{cta_withimage39="/cta-blocks"}} | The Healthcare compliance checklist
7. Streamlined compliance
Achieving compliance with HIPAA will help your organization meet the requirements for other industry standards due to overlapping controls. The opposite is also true—if your organization is compliant with industry-leading frameworks such as HITRUST, SOC 2, NIST, and GDPR, you likely already meet some HIPAA requirements, which can expedite the compliance process.
However, multi-framework compliance also introduces the risk of duplicative workflows. Your teams may lose time and resources reviewing and implementing controls that already meet existing requirements.
You can mitigate this issue by leveraging a centralized compliance tracking solution like Vanta that comes with a cross-mapping feature. This allows your compliance and security teams to cross-reference and map existing controls across frameworks, freeing up time for them to focus on gaps that actually require attention.
How to achieve HIPAA compliance with Vanta
Vanta is an end-to-end trust management platform that streamlines HIPAA compliance by providing guidance and resources across policies, documentation, and control implementation. Depending on your existing tech stack, Vanta can automate up to 85% of HIPAA workflows, saving you time and resources and reducing the risk of human errors that could lead to non-compliance.
The platform offers a dedicated HIPAA product that comes with various helpful features, including:
- Automated evidence collection with 375+ integrations
- A unified dashboard for real-time monitoring
- Pre-built policy templates with an in-app editor
- Ready-to-use document templates
- Built-in governance and training solutions
If you’ve already achieved compliance with industry-standard frameworks like HITRUST, SOC 2, and ISO 27001, Vanta can map your existing controls to HIPAA requirements via its cross-mapping feature. This eliminates duplicative work, saving you significant time and resources while pursuing compliance with multiple frameworks, in an all-in-one solution.
Schedule a custom demo to explore Vanta’s features and see firsthand how it can streamline HIPAA compliance.
{{cta_simple18="/cta-blocks"}} | HIPAA product page
A note from Vanta: Vanta is not a law firm, and this article does not constitute or contain legal advice or create an attorney-client relationship. When determining your obligations and compliance with respect to relevant laws and regulations, you should consult a licensed attorney.

Introduction to HIPAA
7 benefits of HIPAA compliance for your organization

Looking to streamline the work for HIPAA compliance?
The Health Insurance Portability and Accountability Act (HIPAA) is a U.S. federal law that came into force in 1996, with the ultimate goal to establish standards for protecting sensitive patient information. The regulation primarily applies to organizations that handle protected health information (PHI), which refers to a patient’s individually identifiable information collected or generated during treatment.
Since HIPAA compliance is mandatory for many organizations in healthcare, avoiding the related fines is enough of an incentive to invest in compliance.
However, organizations not legally obligated to follow the regulation are also considering compliance. These are organizations looking to enter regulated markets and want to demonstrate optimized security systems or operations to stakeholders or justify the resources HIPAA demands to leadership.
In this guide, we’ll look at seven benefits of pursuing HIPAA compliance—with these, you’ll be able to assess HIPAA’s value for your organization and build a case to get the necessary buy-in from stakeholders.
Who needs to comply with HIPAA and why it matters
Today, any organization that stores, maintains, or transmits PHI must comply with HIPAA.
HIPAA’s original goal was to improve health insurance portability by ensuring that individuals don’t lose coverage between jobs, particularly if they have pre-existing health conditions. Over time, the law has expanded to include federal standards for safeguarding sensitive patient information.
These additional measures put increased financial pressure on insurers, which could be passed on to customers. To address these issues, the Department of Health and Human Services (HHS) established standards aimed at reducing administrative strain and codifying the rules for handling PHI. These rules were originally developed for covered entities, which include:
- Healthcare providers
- Health plans
- Healthcare clearinghouses
The HITECH Act in 2009 broadened HIPAA’s scope to include business associates, which are organizations that enter business associate agreements (BAAs) with covered entities and handle PHI on their behalf.
Organizations that fail to comply with HIPAA can face serious consequences. The HHS Office for Civil Rights (OCR) evaluates violations based on their severity and intent, and may impose different penalties, including corrective actions, financial penalties, or even criminal charges.
7 key benefits of HIPAA compliance
Achieving ongoing HIPAA compliance—mandatory or otherwise—provides several notable benefits to your organization, including:
- Improved security posture
- Enhanced customer trust
- Expanded business opportunities
- Effective risk mitigation
- Improved operational efficiency
- Increased security assurance
- Streamlined compliance
1. Improved security posture
The most significant benefit of HIPAA compliance is an improved security posture. Since HIPAA's core objective is to protect sensitive health information, it requires organizations to implement several key security practices, including:
- Encryption
- Access control
- Data minimization
- Audit trails
HIPAA also strengthens your security posture by enabling rigorous testing and assessments. You'll conduct thorough reviews as part of the preparation process, so you’ll know how effective your security controls are.
The HIPAA Security Rule also emphasizes the need for regular reviews, which you can achieve through continuous monitoring. That way, you’ll be able to stay up-to-date with evolving security practices efficiently, and minimize gaps and non-compliance risk.
Keeping up with regulatory changes becomes particularly important following the 2025 updates to the Security Rule, aimed at making security requirements significantly more prescriptive. Some notable updates include areas such as:
- Risk analysis
- Encryption
- Inventory management
- Multifactor authentication
- Third-party risk management
{{cta_withimage13="/cta-blocks"}} | HIPAA compliance checklist
2. Enhanced customer trust
HIPAA is one of the oldest and most commonly used security standards in the healthcare industry. Demonstrating compliance with it is an effective way of showing your organization’s dedication to data security and privacy, enhancing partner and customer trust.
The framework implements multiple industry-best measures that overlap with several other leading frameworks, such as:
This overlap means that compliance with HIPAA will give you a head start when pursuing other frameworks to enhance customer trust. For instance, you can achieve SOC 2 attestation or NIST certification faster to demonstrate security to a lead and expedite the deal cycle.
3. Expanded business opportunities
HIPAA compliance can be valuable even if you haven’t yet entered the healthcare market or want to explore a new market segment. Demonstrating that you meet all of the regulation’s requirements can help you secure contracts even as a fairly new startup.
HIPAA compliance can also benefit organizations outside the healthcare sector. Aligning with an industry-leading standard can give your organization a competitive edge in other industries where data protection is critical, such as finance, SaaS, or online media.
Additionally, HIPAA may boost your eligibility to win certain government contracts, especially those involving health data or requiring strong privacy practices to protect personally identifiable information (PII). While HIPAA-aligned controls won’t tick off government requirements automatically, they can help streamline the qualification process and demonstrate a strong baseline of security.
4. Effective risk mitigation
Conducting regular risk assessments is a core requirement of continuous HIPAA compliance. Frequent evaluations provide better insights into the effectiveness of your existing controls and help identify potential issues before they escalate.
Proactive measures are particularly important for compliance with the Breach Notification Rule. Under this rule, when a covered entity experiences a security incident involving unsecured PHI, it must notify the HHS and affected individuals within strict timeframes.
Even if your organization isn’t in the healthcare industry, strict breach reporting requirements highlight the importance of taking proactive measures and implementing an effective incident response plan.
Regular assessments will also help you manage third-party risk more effectively. According to HIPAA, you’ll have to consider vendor risk for third parties like business associates as part of your mitigation plans, which helps maintain a clear audit trail.
5. Improved operational efficiency
One of the main ideas behind HIPAA is streamlining operational and administrative processes for covered entities. To achieve this, the framework introduces standardized procedures and protocols under the Security and Privacy rules.
For example, the Privacy Rule requires organizations to implement strict guidelines for disclosing PHI, train employees how to follow them, and share only the minimum amount of information needed for a specific purpose.
The Security Rule focuses on safeguarding electronic PHI by requiring access control, audit logging, and incident response protocols. This rule also specifies the requirements that need to be outlined in business associate agreements, which you can use to streamline your third-party risk management efforts.
Following an established set of controls helps you maintain your security posture efficiently and minimizes the risk of uneven implementation between departments.
6. Increased security assurance
HIPAA does not offer an official certificate for compliance, unlike many other frameworks. As a federal regulation, HIPAA requires all in-scope organizations to comply, regardless of whether they've completed an external audit or assessment.
Organizations looking to demonstrate compliance to third parties can still do so by completing one of two types of assessments:
- Self-assessments conducted by internal teams to evaluate compliance with HIPAA requirements
- Third-party assessments performed by an independent consultant or auditor to provide external validation
Although self-assessments may be more straightforward, an independent auditor brings objective insight on how well your organization has implemented the required controls, providing additional confidence in your security posture.
If your organization handles PHI, you may also be subject to HHS audits. These are performed by the OCR to evaluate whether you meet the requirements for the Security, Privacy, and Breach Notification rules. An audit may happen at random or following a breach or complaint.
HHS audits are enforcement activities—unlike self- and third-party assessments, violations may result in corrective action or fines. That’s why HIPAA specifically mandates compliance-related documentation must be retained for a minimum of six years, as it’s a key part of demonstrating compliance during an HHS audit.
{{cta_withimage39="/cta-blocks"}} | The Healthcare compliance checklist
7. Streamlined compliance
Achieving compliance with HIPAA will help your organization meet the requirements for other industry standards due to overlapping controls. The opposite is also true—if your organization is compliant with industry-leading frameworks such as HITRUST, SOC 2, NIST, and GDPR, you likely already meet some HIPAA requirements, which can expedite the compliance process.
However, multi-framework compliance also introduces the risk of duplicative workflows. Your teams may lose time and resources reviewing and implementing controls that already meet existing requirements.
You can mitigate this issue by leveraging a centralized compliance tracking solution like Vanta that comes with a cross-mapping feature. This allows your compliance and security teams to cross-reference and map existing controls across frameworks, freeing up time for them to focus on gaps that actually require attention.
How to achieve HIPAA compliance with Vanta
Vanta is an end-to-end trust management platform that streamlines HIPAA compliance by providing guidance and resources across policies, documentation, and control implementation. Depending on your existing tech stack, Vanta can automate up to 85% of HIPAA workflows, saving you time and resources and reducing the risk of human errors that could lead to non-compliance.
The platform offers a dedicated HIPAA product that comes with various helpful features, including:
- Automated evidence collection with 375+ integrations
- A unified dashboard for real-time monitoring
- Pre-built policy templates with an in-app editor
- Ready-to-use document templates
- Built-in governance and training solutions
If you’ve already achieved compliance with industry-standard frameworks like HITRUST, SOC 2, and ISO 27001, Vanta can map your existing controls to HIPAA requirements via its cross-mapping feature. This eliminates duplicative work, saving you significant time and resources while pursuing compliance with multiple frameworks, in an all-in-one solution.
Schedule a custom demo to explore Vanta’s features and see firsthand how it can streamline HIPAA compliance.
{{cta_simple18="/cta-blocks"}} | HIPAA product page
A note from Vanta: Vanta is not a law firm, and this article does not constitute or contain legal advice or create an attorney-client relationship. When determining your obligations and compliance with respect to relevant laws and regulations, you should consult a licensed attorney.

Explore more HIPAA articles
Introduction to HIPAA
HIPAA requirements
Preparing for HIPAA compliance
Streamlining HIPAA compliance
Get started with HIPAA:
Start your HIPAA journey with these related resources.

An 8-step HIPAA compliance checklist to meet privacy and security requirements
Use this handy HIPAA compliance checklist to ensure adherence to the key requirements.

HIPAA violations in 2025: Staff mistakes and vendor blind spots
Discover what a HIPAA violation is, common causes behind violations
Live Demo: Automating Compliance for SOC 2, ISO 27001, HIPAA, and More
Discover how Vanta’s automation and AI tools can help your team simplify compliance, strengthen security, and scale trust across frameworks like SOC 2, ISO 27001, HIPAA, and more.




